Abstract
Background: Utilization behaviors in adult sickle cell disease (SCD) patients are driven by a complex mix of factors, which may result in avoidable ED visits and hospitalizations. We partly tested the hypothesis that an intense ambulatory case management program, as part of an Adult Sickle Cell Medical Home that also includes urgent care and inpatient management components, reduces avoidable ED visits and hospitalizations, along with their associated charges. Case management (CM) and community health workers (CHWs) are two evidence-based health management strategies that can help reduce health risks, readmission rates, and improve patient-provider relationships1. In 2019, A DMAIC model2 was published and after four years demonstrates how this program saved money and improved patient satisfaction.
Method: After years of attempting adult SCD CM with two MDs and one advanced practice provider (APP), Virginia Commonwealth University Medical Center (VCU) built upon a pilot study of CM and CHWs and implemented a multi-disciplinary Adult Sickle Cell Medical Home that assigned one of two CHWs for CM of the 50 highest SCD adult utilizers ranked by calendar year (CY) 2017 VCU charges, then by CY 2017 inpatient days1. A PN was assigned to each of the program's top 50 highest utilizers, but also began periodically managing other patients ad hoc in 2019. Activities focused on education to improve self-care, assisting patients with medical appointments, and accessing services to combat adverse social determinants. PNs strove to reduce avoidable (ED) visits and hospitalizations. Interventions and visit activity included telephone, face-to-face clinic, ED, inpatient, or community contact (restricted to telecommunication by COVID). The study sample was Medical Home enrollees from 2011-2021, well before and well after adult program onset. Analyses included: Analysis of Variance (ANOVA), comparing mean annual program ED use, in 2017 (reference group) 2018, 2019, 2020, and 2021 respectively.
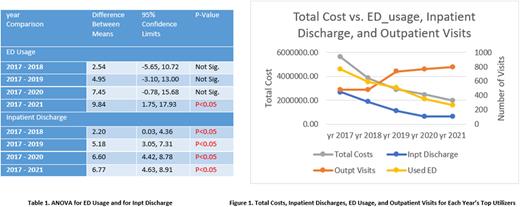
Results: Means of both annual program ED use and annual program inpatient discharges for the top 50 utilizers decreased each year after program onset, compared to 2017, the reference year before program onset (Table 1). Based on inspection of the raw data and suspected COVID effects. ERR for the top utilizers also decreased significantly (ANOVA p-value<0.0001).
Total annual charges correlated with annual Inpatient Discharge (Spearman R=0.67, P-value<0.0001) and ED usage (Spearman R=0.42, P-value<0.0001) from 2017-2021. We managed to decrease the Inpatient Discharge significantly (ANOVA P-value<0.0001) and the ED usage (ANOVA P-value=0.0094) significantly. The increase of ambulatory visits was not statistically significant due to COVID (data not shown).
The impact of the PNs also demonstrates the amount of time, effort and outliers of patient issues contributed to the improvement of patient care and the impact of the financial implications to the institution. Even though the table below doesn't indicate an inverse correlation between time spent on patients and inpatient discharge, and between time spent and ERR, but as a team (with our physicians, RNs, and other team members) we managed to decrease the number of inpatient discharge and ERR.
Conclusion: A proactive and intense ambulatory case management program, as part of an Adult Sickle Cell Medical Home is associated with a reduction year-over-year among top utilizers of total annual charges, ED visits and hospitalizations, as well as an increase in ambulatory visits. The hands on, personal team approach will continuously provide results indicative of patients' lives being improved, plus avoided or reduced costs are also providing financial relief to the hospital system.
Disclosures
Smith:Agios: Research Funding; Global Blood Therapeutics: Consultancy, Honoraria, Research Funding, Speakers Bureau; Emmaus: Consultancy; Forma Therapeutics: Consultancy, Research Funding; Novo Nordisk: Other: DSMB; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Research Funding; Imara: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal